In many countries where we work, the COVID-19 pandemic has overburdened healthcare systems that were already ill-equipped to care for extremely sick people. The health system in South Sudan is one such example. However, our work to establish an infectious disease unit (IDU)—which became home to South Sudan’s first and only Level 1 intensive care unit (ICU)—has helped the country better prepare itself to take care of its sickest patients.
The WHO and South Sudan’s Ministry of Health built the Dr. John Garang Infectious Disease Unit in Juba in late 2018 to prepare for the possibility of an Ebola outbreak, as the disease raged in the neighboring Democratic Republic of the Congo. The IDU was meant to serve as an isolation facility where Ebola patients could be diagnosed and treated while the country opened additional treatment centers. Originally imagined as a temporary facility, the government quickly decided to build the IDU as a semi-permanent structure that could be used in the future to treat other infectious diseases. This turned out to be a prescient decision.
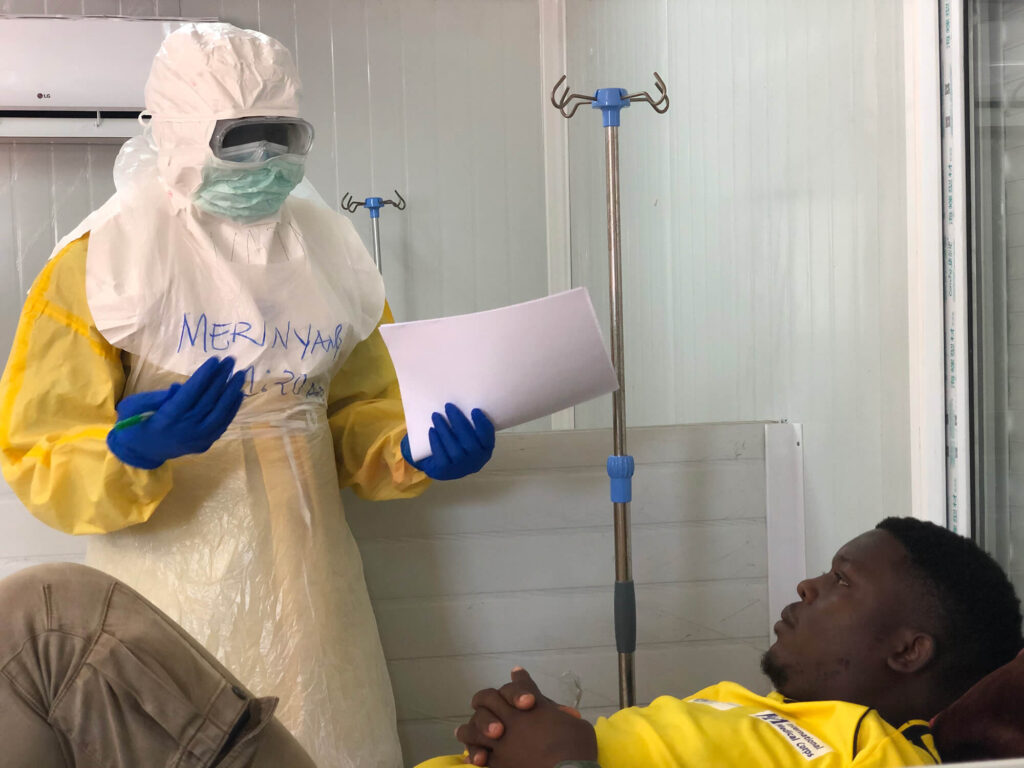
Because it lacked resources to operate the facility, the Ministry of Health handed over operation of the IDU to International Medical Corps in February 2019. Dr. Abdou Sebushishe, who today serves as our Acting Country Director in South Sudan, joined International Medical Corps the following month, charged with operating the unit, putting guidelines in place to manage the prevention of infectious disease and training staff in infection prevention and control (IPC) measures.
Fortunately, Ebola never materialized in South Sudan—though the unit did admit 23 suspected patients who later tested negative. In early 2020, however, as International Medical Corps was preparing to hand the unit back over to the Ministry of Health, the country was suddenly faced with a new challenge: COVID-19. The Ministry of Health requested that we stay at the IDU and maintain the same level of operations for the new outbreak.
That spring, we received the funding necessary to increase the level of care that the IDU could provide, upgrading from an isolation unit to an infectious disease treatment facility. Still, we were able only to provide minimal support to patients: monitoring them, and providing fluids, basic treatments and medications. We did the best we could, bringing in the additional resources, drugs and equipment that were needed until November 2020, when the Ministry of Health requested that our Emergency Medical Team (EMT) increase the level of care at the IDU even further.
The EMT sent five critical-care specialists to the IDU: a team lead, an ICU nurse, an ICU physician with a background in anesthesia and critical care medicine, an ICU physician trained in point-of-care diagnosis, and a biomedical engineer who could review the unit’s equipment.
“The EMT started from scratch, doing an assessment of the critical-care capacity in South Sudan,” Dr. Abdou explains. The report found low capabilities for critical care in South Sudan and made a number of recommendations. “We started implementing those recommendations to increase capacity in the IDU to a Level 1 intensive care unit,” he says.
Today, the eight-bed Level 1 ICU enables critical-care workers to provide additional medical support to patients who are very ill. It has been equipped with sophisticated, real-time monitoring equipment, ventilators and supplementary oxygen devices. Health staff can use a new point-of-care laboratory to check blood hemoglobin or protein levels in urine, or to test people for diseases such as HIV or malaria.
“We now have a Level 1 ICU—the first ever in South Sudan that is accessible to the general public—where everyone can go, and which everyone can rely on,” says Dr. Abdou. “It has made a very big difference, and it has brought hope that South Sudan can start thinking about how to expand critical-care capacity. That is a big impact for the future of the health system in this country—and that was brought about by the IDU and 100% supported by International Medical Corps.”
As part of the EMT’s plan, IDU staff also have conducted training sessions for healthcare workers on topics including life support, ultrasound use, and the diagnosis and treatment of common illnesses requiring critical care, including COVID-19.
It isn’t just the trainees who’ve benefited, however; the sessions also function as learning opportunities for the trainers themselves. “We make sure to take advantage of any opportunity to conduct training, so that our training staff are getting used to the systems and remaining up to date on procedures,” Dr. Abdou points out.
So far, 268 patients have been admitted to the 82-bed IDU facility, which has the capacity to expand to 250 beds if necessary. Fortunately, the IDU has never admitted more than 21 patients at a time, though it stands at the ready should the need arise. New funding will keep the IDU open as the delta variant spreads and COVID cases increase.
“We are prepared for this new resurgence,” says Dr. Abdou. “Our staff are trained and ready; our equipment is functional. We also have a roster so that we can quickly scale up to the 250-bed potential of the ICU while providing good services to the people, if needed.”
